For more than 30 years, newly diagnosed patients with IC/BPS were given bladder medications with little, if any, success. Why? Researchers and clinicians believed, at that time, that IC was an incurable bladder disease. Today, that perception has changed dramatically. Our updated 2022 AUA Guidelines for IC/BPS very clearly state that no active “disease” is actually found in the vast majority of IC patients.(1) They now believe that patients are struggling with a pelvic pain syndrome driven by dysfunctional nerves and/or muscles. For the patient, though, finding the correct treatment for their unique case of IC/BPS is challenging. Phenotyping (aka subtyping) helps find the most effective treatments.
For the past six years, we’ve embraced the system proposed by Dr. Christopher Payne.(2) He believed that there are five core patient groups, each requiring their own unique treatment including: Hunner’s lesion, Bladder Wall Driven (chemocystitis, estrogen atrophy, etc.), Pelvic floor Driven, Pudendal Neuralgia and Central Sensitization/Chronic Overlapping Pain Conditions. Yet, in his proposal, he also suggested that more subtypes could emerge.
The American Urology Association guidelines now recognize that there are at least three distinct patient groups: bladder wall (Hunner’s lesion, chemocystitis, estrogen atrophy, chronic UTI), pelvic floor driven and central sensitization/widespread pain. Last fall, during a critical meeting held by the National Institutes of Health (NIDDK) on future IC research, researchers around the world agreed that there are distinct patient groups, with a clear admission that previous studies failed because they put diverse patients into the same studies.
From this point forward, the new approach to IC/BPS treatment focuses on “precision medicine” in which treatments must be selected AFTER the patient subtypes have been identified. The goal? To find the most effective treatment for each unique patient.
Focus on Individualized Treatment

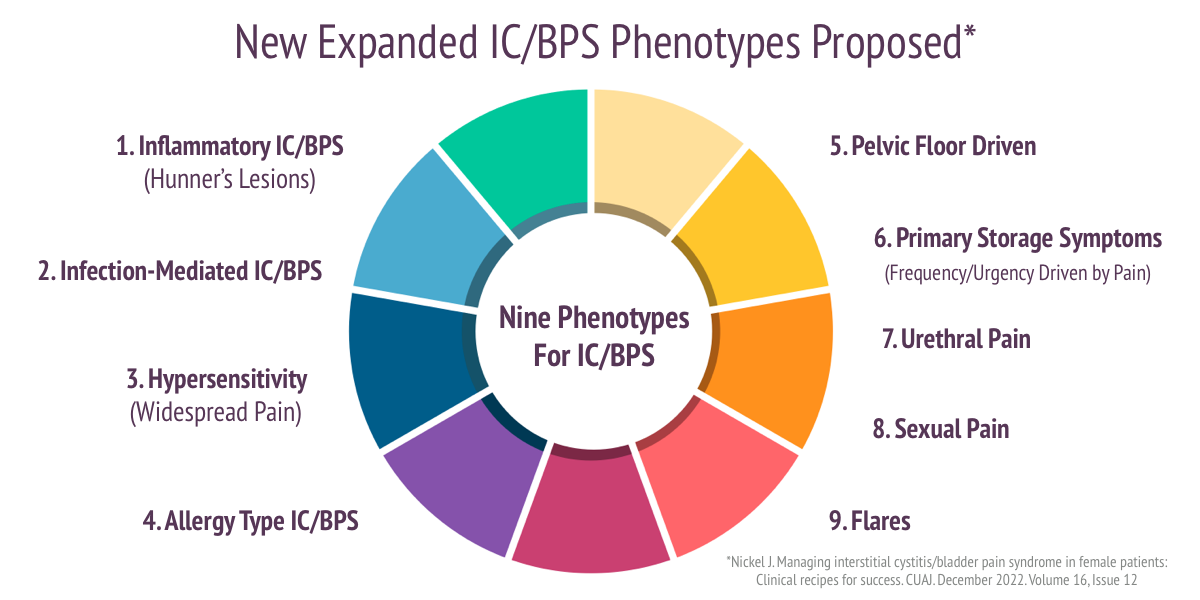
Curtis Nickel
Dr. Curtis Nickel, the pre-eminent IC researcher and clinician in Canada, offers a new proposal of nine potential phenotypes/subtypes found within the IC/BPS patient community.(3) He wrote ‘I have been asked by urologists many times over the decades how to treat a specific patient with IC/BPS and found that I gave a different answer based on…. each patients “clinical picture.”‘ He has found that “a stepwise, mono therapy approach… is doomed for failure in the majority of patients suffering from IC/BPS.”
Dr. Nickel’s credentials are impeccable. He has conducted 24 clinical trials, conducted over 200 IC studies, written or contributed to over 600 publications, presented courses in over 45 countries and, as a Professor at Queens University, has worked with hundreds of patients over the years. He is also a former president of the Canadian Urological Association.
Dr. Nickel uses the concept of a recipe to describe a patient treatment plan. Each recipe begins with some common ingredients. He encourages patients to be willing to learn about IC/BPS and to be proactive with their diet and exercise. Eliminating foods that are known triggers is an easy first step. To trigger the production of endorphins (natural pain killers), low impact exercises (walking, swimming, elliptical) are suggested with a caution to avoid exercises that put pressure on the perineum (i.e. biking). Positive mind exercises (positivity, mindfulness) help in healing and improved outcomes over time. Because anxiety, depression and catastrophizing can worsen pain and quality of life, patients should be willing to seek support whether it be from their doctor or a psychologist.
To physicians, he reports using DMSO and Elmiron® less frequently due to both short and long-term risks, such as retinal disease. He encourages the use of pain management EARLY in all patients, including: NSAIDs, acetaminophen, urinary analgesics. He believes that the long-term use of opioids should be avoided because they restrict the bodies own natural opioid production and fail to provide pain benefit over time. He notes, however, that the strategic use of cannabis seems to help patients cope better. We would add the very affordable OTC supplement palmitoylethanolamide (PEAORA®) to this regimen based upon the 2019 IC/BPS study which found success in reducing pain and discomfort.(4)
Dr. Nickel wrote “It is imperative that pain outside the pelvis associated with IBS, fibromyalgia, chronic fatigue syndrome, back pain be managed.” Pain left untreated acts to “up-regulate” the nervous system, making it more sensitive to pain. This may require multiple specialists including a urologist, gastroenterologist, gynecologist, rheumatologist, physiotherapist, etc.
Surgery is the very last result and only for patients who have tried all other therapies with no success and/or have an end-stage bladder (a bladder that has lost its ability to expand to hold urine and may be fibrotic).
Lastly, he established a nurse based intravesical treatment clinic on Friday afternoons for regular treatment and, if necessary, for flare management noting that flares seem to occur more frequently just before the weekend.
Nine Subtypes & Their Treatment Recipes
1. Inflammatory IC/BPS
This subtype includes patients who have visible inflammation on their bladder or Hunner’s lesions. If lesions are present, Dr. Nickel suggests that they should be cauterized, multiple times if necessary. After successful treatment with cauterization, Dr. Nickel switched to steroid injections (triamcinolone) into the lesion with the total dose not exceeding 80 mg. For early or mild recurrences, he suggests using a classic rescue instillation containing lidocaine, triamcinolone, and either chondroitin sulfate, heparin sulfate or sodium hyaluronate. For patients who do not respond to these treatment, oral cyclosporine has been successful.
2. Infection-mediated IC/BPS
This is a new subtype that no other system recognizes. Dr. Nickel argues that there are patients who have a history of recurring UTI”s may be experiencing a “bladder hypersensitivity syndrome” secondary to the infection. While long-term antibiotic therapy is an option, Dr. Nickel suggests applying antibiotics directly to the bladder via bladder instillation. He also shares the results of research with a new vaccine (MV140) which their study showed significantly reduced UTI’s.(4) He believes that the future of testing to identify UTI is next generation DNA urine testing though future research is still needed.
3. Neurogenic hypersensitivity IC/BPS
These patients have multiple widespread pain conditions, such as IBS and fibromyalgia. Known as chronic overlapping pain conditions or central sensitization, the goal of therapy is to calm the nerves in the bladder wall and central nervous system. These patients may benefit from the use of low dose antidepressants (amitriptyline) and bladder instillations that the support the GAG layer (chondroitin sulfate, heparin sulfate, sodium hyaluronate). If pain is present, the addition of lidocaine to the instillation is suggested.
4. Multiple Allergies IC/BPS
These patients struggle with respiratory, environmental and/or dietary allergies. He says they can be easily identified during a cystoscopy by gently poking the bladder wall with the tip of a flexible cystoscope to look for a “mucosal wheal-flare reaction.” He suggests that these patients should follow a strict diet and use an antihistamine (hydroxzyine) and/or cimetidine. The patients may also benefit from a typical rescue instillation.
5. Pelvic Floor Pain
Patients demonstrating pelvic floor dysfunction, tension and/or trigger points, will benefit from therapies that target muscle health, including: localized heat, stretching, relaxation, physical therapy and the use of skeletal muscle relaxants (i.e. diazepam vaginal suppository 10mg). “It is imperative that pelvic floor physical physiotherapy be undertaken by specialists trained in pelvic floor manipulation,” he suggested. If pain is localized to one side and/or appears to follow nerve pathways, nerve blocks may be necessary. Pelvic floor BotoxA therapy may also be helpful though he did not use this in his clinic.
6. Primary Storage Symptom Syndrome
Some IC/BPS patients run to the restroom to reduce pain. Their frequency and urgency is driven by avoiding the pain caused by bladder filling. Dr. Nickel believes that these patients can benefit from an antimuscarinic medication (solifenacin) if pain has first been controlled. Mirabegron helps patients with both urgency/frequency and pain. He believes that bladder training is essential to increase bladder capacity. “As a last resort, BotoxA can provide short-term symptom relief though it carries a risk of urinary retention,” he offered. Sacral neuromodulation has helped some patients but Dr. Nickel did not believe that it significantly improved pain.
7. Urethral Pain Syndrome
This new subtype is, in Dr. Nickel’s opinion, one of the most difficult to help. These patients have pain in the urethra, sometimes as their only symptom. It can be constant, episodic or associated with urination. Treatment can include topical lidocaine (2-5% gel) to numb the urethra, vaginal estrogen to improve skin health, local or oral amitryptiline, phenazopyridine, diazepam and/or a periurethral block.
8. Associated Sexual Pain
Pain with intimacy must be addressed in patients who are sexually active. The location of the pain must first be assessed. Is it coming from the vagina, vulva, pelvic floor or bladder? Pelvic floor physical therapy, topical lidocaine and estrogen therapy to improve vaginal skin health is a priority.
9. IC Flares
Patients struggling with a sudden worsening of their symptoms need additional care. Flares can be triggered by diet, menstruation, stress, other infections, inflammatory or painful conditions and intimacy. Flares can last for a few hours to several days. If flares correspond with menstruation, hormone therapy may be suggested. Common flare management strategies include:
- diet modification
- increasing water intake
- stopping irritating vitamins or supplements (i.e. cranberry, multivitamins with vitamin C, etc.)
- stress reduction
- using heat or cold compresses
- short term antihistamines.
- phenazopyridine,
Conclusion
Dr. Nickel’s system is quite complementary to Dr. Payne’s five subtypes. By offering yet more diversity, such as the allergy and/or urethra subtypes, it will help both patients and providers find more accurate and effective therapies. And, as he notes, there may be more variants yet to be discovered, such as a subtype associated with autoimmune dysfunction (i.e. Sjogren’s, Lupus).
It’s wonderful to see our best and most experienced researchers and clinicians leaving a legacy that will help the next generation. From Dr. Jerome Weiss’s fabulous book “Breaking Through Chronic Pelvic Pain” to this work, we are seeing tremendous change and growth in the IC/BPS world. The future looks more promising than ever.
You, the IC patient, can play an important role in making these changes happen. Please bring this article to your urologists, urogynecologists, ob-gyns and primary care providers who, admittedly, are unlikely to read the Canadian Journal of Urology. The concepts are sound and we must help physicians in the USA and around the world adopt these principles.
References:
- Clemens JQ, Erickson DR, Varela NP et al: Diagnosis and treatment of interstitial cystitis/bladder pain syndrome. J Urol 2022; https://doi.org/10.1097/JU.0000000000002756.
- Payne C. A New Approach To Urologic Chronic Pelvic Pain Syndromes: Applying Oncologic Principles To ‘Benign’ Conditions. Current Bladder Dysfunct Rep. Topical Collection on Pelvic Pain. March 2015
- Nickel J. Managing interstitial cystitis/bladder pain syndrome in female patients: Clinical recipes for success. CUAJ. December 2022. Volume 16, Issue 12
- Cervigni M, et al. Micronized Palmitoylethanolamide-Polydatin Reduces the Painful Symptomatology in Patients with Interstitial Cystitis/Bladder Pain Syndrome. Biomed Res Int. 2019; 9828397.
- Osborne J. Uromune Vaccine To Prevent UTI Showing Remarkable Success. ICN. February 19, 2022