If commuting or taking long car rides exacerbates your bladder or pelvic pain symptoms, you are not alone. The first epidemiological studies on IC found that 50% of patients reported pain and discomfort while sitting in a car.(1) The vibration from bumpy roads, as well as constant starts and stops, are jarring to the bladder and pelvic floor muscles. Throw in restricted restroom access and/or the perception that a restroom might not be available, it’s only natural that patients find rides stressful and unenjoyable. Fear not! Here are some strategies that can help:
A smooth suspension is a must

After my IC/BPS began, I spent a year test driving cars, SUV’s and trucks in search of one that didn’t make me cry. The most comfortable were mid to larger SUV’s and sedans which, given todays’ gas prices, seems daunting. Some car brands (i.e. Buick, Kia) are known for having smoother suspensions. I drove a midsize Buick Rendezvous for many years and it was perfect for my tender bladder and pelvic floor. The seats were soft, comfortable and supportive. I barely felt bumps in the roads or on the freeways. Smooth as silk! After 13 years, it eventually died and I switched to the smaller Nissan Rogue. While it’s not quite as good as the Buick, the seats work and the drive is pretty smooth. Fair warning. It does have a lot more road noise. I hope to update to a Nissan Pathfinder later this year (if prices go down) which has more storage capacity because I often have to evacuate due to fires.
When in doubt, try renting a car that seems promising for a few days. You need more time than a typical test drive. You’ll want to drive throughout your neighborhood and nearby streets and highways to see if it’s truly comfortable and will work for you.
Going on a train ride?
If you’re planning a long train trip, consider upgrading to Business or First class which have better suspensions and more comfortable seats. I had one of my worst flares ever and ended up in the Emergency Room after riding in the cheap seats on Amtrak for a five hour trip. Never again!
Bring a Restroom Access Card
If you’re worried that you’ll be denied access to a restroom, try showing an ICN Restroom Access card. These come in handy in any situation where restroom access might be limited, including plane flights, train rides and private facilities. Of course, you’ll find some of the best bathrooms off the freeway at Starbucks, McDonald’s and other fast food restaurants.
Try using a Bladder & Pelvic Friendly Chair Cushion

Some seats are too hard, too firm or just put pressure exactly where you are the most sensitive. Donut shaped pillows don’t work because they put pressure on your urethra and stretch the perineum awkwardly. The ICN offers the innovative Pelvic Pain Chair Cushions that reduce pressure on your urethra, vulva, scrotum and/or rectum and are much more comfortable. If you struggle with pelvic floor tension, especially your glutei muscles, our Waffle Chair Cushion is ideal.
Carry TravelJohns
Some patients allow themselves to become housebound because they worry that they will not be able to find a restroom or, worse, get stuck in a traffic jam. Try carrying some TravelJohns, an ingenious portable urinal for men and women that is small enough to fit in your purse, glove compartment or pants pocket. In fact, I always have a handful in my car for emergencies! Each contains a small, yet strong plastic bag that fits perfectly over your tender bits. When you urinate into them, a chemical instantly solidifies the liquid it to avoid leakage. Simply throw away in any trash can. These are ideal for planes, trains and cars!
The Sunany or Tinkle Bell Female Urination Device allow women to pee standing up so that you can avoid nasty or dirty bathroom seats.
Some patients just keep beach towels and thick plastic bags in their car. Put the towel in the bag, sit and go. Seal with a twist tie and then wash at your earliest opportunity. Others make sure that they drive a four door car. They open the back door and the front door, to create a private area for emptying their bladder by the side of the road. There ARE ways!
Try using a TENS unit during the drive
 Under no circumstance should an IC patient drive while taking strong or sedating medications. You risk not only your health, but those of other drivers by driving impaired. If pain is an issue, consider using a TENS Unit during the drive. In my early years, when driving was especially hard, I would GENTLY slap my thigh while driving. This acts similarly to a TENS unit and diverted my attention away from the pain. Having the actual device, which delivers mild, electrical stimuli to the muscles of your thighs, lower abdomen or back may help. Please ask your physical therapist and/or physician for guidance on how to use the device, the correct settings and placement of the pads.
Under no circumstance should an IC patient drive while taking strong or sedating medications. You risk not only your health, but those of other drivers by driving impaired. If pain is an issue, consider using a TENS Unit during the drive. In my early years, when driving was especially hard, I would GENTLY slap my thigh while driving. This acts similarly to a TENS unit and diverted my attention away from the pain. Having the actual device, which delivers mild, electrical stimuli to the muscles of your thighs, lower abdomen or back may help. Please ask your physical therapist and/or physician for guidance on how to use the device, the correct settings and placement of the pads.
Use BodiHeat heating pads!

A heating pad helps to relax muscles that often begin tightening on long car rides or plane flights. I love the Beyond BodiHeat adhesive pads because they deliver constant steady heat and can be worn in the car, at work and on planes. The pads are 4″ by 5″ and flat. Simply peel off the adhesive on the back and attach to your underwear. (Never attach to your skin as they can burn.) No-one will ever know you are wearing a heating pad and it may last for up to 8 hours. It does take about 30 minutes to slowly heat up. When finished, do NOT throw into a trash can until cool. I place mine on my bathroom counter overnight.
Treat your body kindly
You would not run a marathon on a broken leg, so try not to run a marathon on a painful bladder or pelvic floor. If you are in an active flare, rest frequently and keep your drives short. There may be times when you should not get in the car, especially for longer car rides or vacations. Assess your pain that morning. If you are in a major flare, it may be best to pass on that car trip knowing that the vibration will probably make you much more uncomfortable by the end of the trip. Many patients report ruined vacations because they sat in the car far too long.
References:
(1) 5. Ho N, Koziol J, Parsons CL. Epidemiology of Interstitial Cystitis, in G. Sant (Ed.), Interstitial Cystitis.Philadelphia: Lippincott-Raven Publishers, 1997; 9-15 9.
Edited – June 8, 2022 – JHO


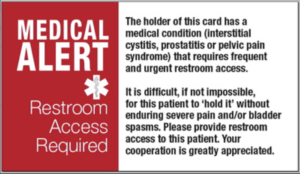

When I take a vacation trip these suggestions work for me: a vehicle with great suspension, chair cushion which I use off and on during the trip, wear a denim skirt with no panties – that way I am not sitting on a seam in jeans or other pants, and an area in the back of the vehicle where I can lie down on my back with my feet elevated. This takes all the pressure off my bladder and usually leads to a short nap. Also have Medical Access Card which was helpful when we flew to Alaska two years ago. And last but not least, an understanding husband who stops for a potty break anytime I need it.
I use Depends. They are good for three uses. I do this for car trips, bike rides, movies, meetings, etc. The first few times, I cried. But now I see it as a way to enjoy my life. I wish I had started using them earlier. If money is an issue, I find them at St. Vincent de Paul, etc, cheap.