IC Subtypes & Phenotypes
Spend anytime in an IC support group and you learn, very quickly, that patients are often very different. Some patients struggle high levels of pain while others have only frequency or urgency. 5 to 10% of patients Hunner’s lesions while others have normal, healthy bladder walls. A whopping 85% of IC patients have tight, dysfunctional pelvic floor muscles while a smaller group of patients struggle with related pain conditions (irritable bowel syndrome, vulvodynia, prostatodynia, fibromyalgia, etc.). In 2023 and beyond, we will be focusing on “precision medicine” in which you, the patient, should be given treatments based upon your unique case and symptoms. This section discusses the diversity, phenotypes and/or subtypes now widely accepted in the IC patient population.
Ulcerative Vs. Nonulcerative
Clinicians around the world agree that the two most obvious subtypes are:
- Hunner’s Lesions – Roughly 5 to 10% of patients have Hunner’s lesions on their bladder wall. This is known as “classic IC.”
- Non-Ulcerative – The remaining 90% of patients often have a normal bladder yet struggle with often profound symptoms.
But this doesn’t help patients and/or doctors select the best treatments unless, of course, they have Hunner’s lesions. What about the remaining 90%? Clearly, they aren’t all identical. Researchers have been working for years to create a more accurate subtyping system.
AUA Subtypes of IC/BPS
In 2022, the American Urological Association released new, updated guidelines for IC/BPS in which they clearly state that IC is NOT a bladder disease, but rather a neuromuscular disorder in the majority of patients.(1) They identified three unique groups:
- Bladder Centric – These patients have a clear dysfunction of the bladder wall, as demonstrated by the presence of Hunner’s Lesions, chronic UTI or Genitourinary Syndrome of Menopause.
- Pelvic Floor – These patients have demonstrated hypertonicity (aka tension) of their bladder wall and should immediately be referred for proper pelvic floor physical therapy
- Chronic Overlapping Pain Conditions – These patients struggle with multiple pain conditions such as: IC, IBS, vulvodynia, fibromyalgia, migraines, TMJ, etc. Research strongly suggests that the central nervous system is dysfunctional (aka maladaptive) and driving nerve sensitivity throughout the body. Therapies focus on calming the central nervous system.
While we were delighted to finally see this change, it was Dr. Christopher Payne’s five point system released in 2015 that first helped both patients and practitioners differentiate between the many potential causes of bladder pain, which we continue to use today. The AUA system is not as specific as the Payne system.
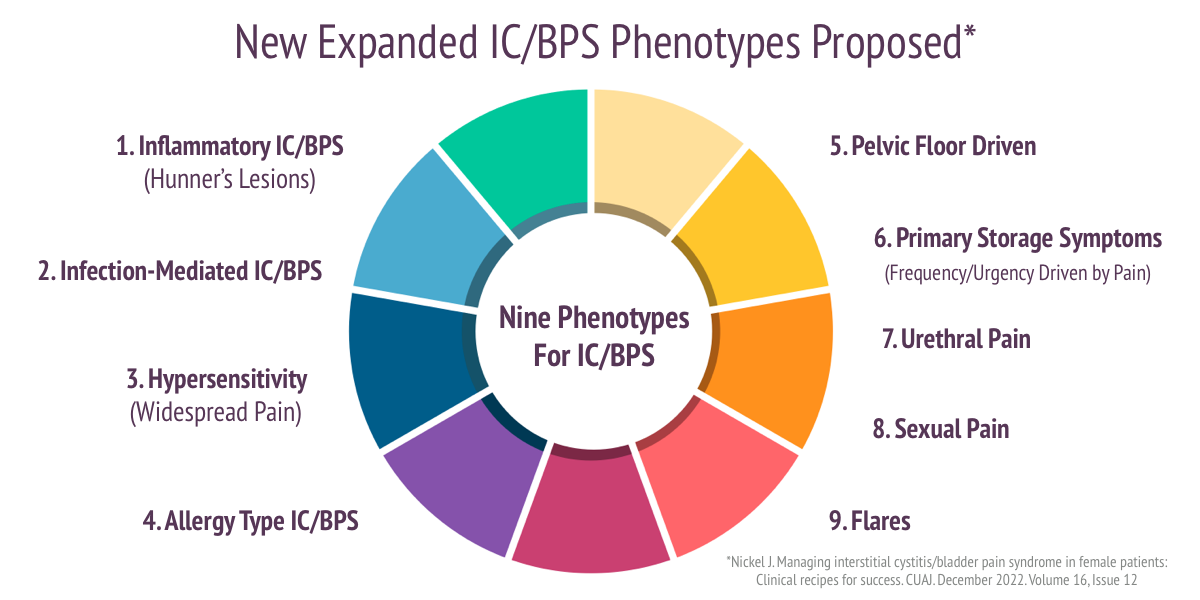
Nine Phenotypes of IC/BPS
In late 2022, Dr. Curtis Nickel, the pre-eminent IC researcher and clinician in Canada, offered a new proposal of nine potential phenotypes/subtypes found within the IC/BPS patient community.(2) He wrote ‘I have been asked by urologists many times over the decades how to treat a specific patient with IC/BPS and found that I gave a different answer based on…. each patients “clinical picture.”‘ He has found that “a stepwise, mono therapy approach… is doomed for failure in the majority of patients suffering from IC/BPS.”
- Inflammatory IC/BPS – This subtype includes patients who have visible inflammation on their bladder or Hunner’s lesions. If lesions are present, Dr. Nickel suggests that they should be cauterized, multiple times if necessary. After successful treatment with cauterization, Dr. Nickel switched to steroid injections (triamcinolone) into the lesion with the total dose not exceeding 80 mg. For early or mild recurrences, he suggests using a classic rescue instillation containing lidocaine, triamcinolone, and either chondroitin sulfate, heparin sulfate or sodium hyaluronate. For patients who do not respond to these treatment, oral cyclosporine has been successful.
- Infection-mediated IC/BPS – This is a new subtype that no other system recognizes. Dr. Nickel argues that there are patients who have a history of recurring UTI”s may be experiencing a “bladder hypersensitivity syndrome” secondary to the infection. While long-term antibiotic therapy is an option, Dr. Nickel suggests applying antibiotics directly to the bladder via bladder instillation. He also shares the results of research with a new vaccine (MV140) which their study showed significantly reduced UTI’s.(4) He believes that the future of testing to identify UTI is next generation DNA urine testing though future research is still needed.
- Neurogenic hypersensitivity IC/BPS – These patients have multiple widespread pain conditions, such as IBS and fibromyalgia. Known as chronic overlapping pain conditions or central sensitization, the goal of therapy is to calm the nerves in the bladder wall and central nervous system. These patients may benefit from the use of low dose antidepressants (amitriptyline) and bladder instillations that the support the GAG layer (chondroitin sulfate, heparin sulfate, sodium hyaluronate). If pain is present, the addition of lidocaine to the instillation is suggested.
- Multiple Allergies IC/BPS – These patients struggle with respiratory, environmental and dietary allergies. He says they can be easily identified during a cystoscopy by gently poking the bladder wall with the tip of a flexible cystoscope to look for a “mucosal wheal-flare reaction.” He suggests that these patients should follow a strict diet and use an antihistamine (hydroxzyine) and/or cimetidine. The patients may also benefit from a typical rescue instillation.
- Pelvic Floor Pain – Patients demonstrating pelvic floor dysfunction, tension and/or trigger points, will benefit from therapies that target muscle health, including: localized heat, stretching, relaxation, physical therapy and the use of skeletal muscle relaxants (i.e. diazepam vaginal suppository 10mg). “It is imperative that pelvic floor physical physiotherapy be undertaken by specialists trained in pelvic floor manipulation,” he suggested. If pain is localized to one side and/or appears to follow nerve pathways, nerve blocks may be necessary, performed by specialists if necessary. Pelvic floor BotoxA therapy may also be helpful though he did not use this in his clinic.
- Primary Storage Symptom Syndrome – Some IC/BPS patients run to the restroom to reduce pain. Their frequency and urgency is driven by avoiding the pain caused by bladder filling. Dr. Nickel believes that these patients can benefit from an antimuscarinic medication (solifenacin) if pain has first been controlled. Mirabegron helps patients with both urgency/frequency and pain. He believes that bladder training is essential to increase bladder capacity. “As a last resort, BotoxA can provide short-term symptom relief though it carries a risk of urinary retention,” he offered. Sacral neuromodulation has helped some patients but Dr. Nickel did not believe that it significantly improved pain.
- Urethral Pain Syndrome – This new subtype is, in Dr. Nickel’s opinion, one of the most difficult to help. These patients have pain in the urethra, sometimes as their only symptom. It can be constant, episodic or associated with urination. Treatment can include topical lidocaine (2-5% gel) to numb the urethra, vaginal estrogen to improve skin health, local or oral amitryptiline, phenazopyridine, diazepam and/or a periurethral block.
- Associated Sexual Pain – Pain with intimacy must be addressed in patients who are sexually active. The location of the pain must first be assessed. Is it coming from the vagina, vulva, pelvic floor or bladder? Pelvic floor physical therapy, topical lidocaine and estrogen therapy to improve vaginal skin health is a priority.
- IC Flares – Patients struggling with a sudden worsening of their symptoms need additional care. Flares can be triggered by diet, menstruation, stress, other infections, inflammatory or painful conditions and intimacy. Flares can last for a few hours to several days. If flares correspond with menstruation, hormone therapy may be suggested. Common flare management strategies include: diet modification, increasing water intake, stopping irritating vitamins or supplements (i.e. cranberry, multivitamins with vitamin C, etc.), stress reduction, using heat or cold compresses, short term antihistamines, phenazopyridine (AZO Bladder Pain Relief Tablets).
The Original Five Subtypes of IC
 In 2015, Dr. Christopher Payne argued that the diagnosis of IC should be much more specific so that a clear treatment pathway can be identified. He suggested five subtypes of IC that assess the whole patient and produces a customized treatment plan(3).
In 2015, Dr. Christopher Payne argued that the diagnosis of IC should be much more specific so that a clear treatment pathway can be identified. He suggested five subtypes of IC that assess the whole patient and produces a customized treatment plan(3).
We use this system in our patient coaching sessions. Be warned, many if not most urologists aren’t aware of any of the subtyping systems.
- IC: Hunner’s lesions – This small subset of patients (10% of the patient population) have inflammatory lesions visible on their bladder wall. In much of the world, only patients with Hunner’s lesions are diagnosed with “interstitial cystitis.” Patients without lesions are diagnosed with “bladder pain syndrome.” Hunner’s lesions require local lesion directed therapy (laser, fulguration, steroid injections) and do not generally respond to oral medications and bladder instillations. A new medical device currently under study, LiRIS (aka LiNKA) is the first treatment in history that has healed and/or reduced the size of lesions in just a two week treatment period.
- BPS: Bladder Wall Phenotype – Patient symptoms often start with a UTI, chemotherapy, chemical exposure or other bladder insult (i.e. drinking excessive amounts of soda, coffee, etc.). Frequency and urgency can occur throughout the day and night. Estrogen atrophy can also influence bladder wall function and sensitivity. Pain increases as the bladder fills with urine and is reduced on emptying. These patients usually find that their pain decreases when an anesthetic (lidocaine) is instilled into the bladder. Treatment priority focuses on calming and soothing the bladder wall, diet modification, OTC supplements, oral medications and other bladder directed therapies.
- BPS: Myofascial Pain Phenotype – These patients often have a history of sports, orthopedic injuries or childbirth trauma. Upon examination, they have pelvic floor tension and the presence of trigger points in their pelvis, abdomen, back and hips that trigger severe symptoms when touched. They may have less diet sensitivity, normal or larger voids, may sleep more comfortably when their muscles are relaxed. Bladder instillation of lidocaine is NOT generally helpful. Treatment priority is pelvic floor physical therapy.
- BPS: Neuralgia Phenotype – These patients can have pelvic floor muscle tension or other causes of pudendal nerve compression. This causes severe burning or electric pain when sitting, “sensory abnormalities in the pudendal distribution” and a positive Tinel’s sign (tingling or pins and needles when the nerve is tapped gently). Pain is not typically linked to bladder function. Treatment starts with identifying causes of injury/irritation, physical therapy and stretching for tight muscles and analgesics specific for neuropathic pain. Nerve blocks can be both diagnostic and therapeutic when conservative measures fail. Surgical nerve release is infrequently needed but can be effective in carefully selected patients.
- Chronic Overlapping Pain Disorders/ Central Sensitization – These patients have multiple pain disorders (i.e. IBS, vulvodynia, fibromyalgia, etc.). Dr. Payne wrote “Their prognosis is inherently different and the invasive treatments that may be appropriate for pelvic pain phenotypes could actually make things worse…Clinicians should proceed much more cautiously.” These patients demonstrate clear signs of nerve sensitization throughout their body, including: extremely sensitive skin, diet sensitivity, drug sensitivity, chemical sensitivity and even visual sensitivity. Most also have an extremely sensitive sense of smell. Treatment priorities focus on calming the “wound up” nerves throughout the body. Treating all pain generators to reduce the overall volume of pain in the nervous system is important. Patients are also encouraged to try Mind-Body therapies that help “wind down” the nervous system, including: progressive relaxation, mindfulness, and, most importantly, anxiety management. Untreated anxiety and catastrophizing actively “winds up” the nervous system and contributes to even greater levels of pain. At no point is anyone suggestion that this is a mental. Rather, it is a nerve and/or nervous system that has been traumatized. The goal of therapy is to restore proper nerve function by reducing painful stimulation and stress.
Dr. Payne’s 2017 Presentation On His Five Point System: “The Emperor has no clothes.”
Hear from Dr. Payne why he created this system, what motivated him and how each subtype can be treated. This is an excellent presentation particularly for medical care providers and nursing staff.
UPOINT
Released in 2009, the second proposed subtyping system was the UPOINT System for the Clinical Phenotyping of Chronic Pelvic Pain by Nickel, Shoskes and Rackley. (4) They asked physicians to look at and beyond the bladder in six different areas, including:
- what bladder symptoms are present?
- what’s the condition of the bladder (i.e. Hunner’s lesions)?
- does the patient have other related conditions (i.e. IBS)?
- what is the health of the pelvic floor muscles?
- does the patient struggle with anxiety / depression?
- has any infection been found?
Based upon the answers to these questions, doctors could then create a custom treatment plan for each patient. This “whole body” approach has been validated in multiple research studies and serves as the foundation for the Canada Urology Associations Guidelines For IC/BPS that were released in 2016.
INPUT
UPOINT has been remarkably helpful when assessing the chronic prostatitis population however for IC, it has key limits because most IC patients have some degree of bladder symptoms and bladder wall dysfunction. Original co-author Dan Shoskes and colleagues have adapted these guidelines to create a new system for use specifically with IC, called INPUT(5). This asks physicians to assess five distinct areas:
- I – Is any infection present?
- N – Does the patient also have any other neurologic or systemic conditions
- P – Does the patient have any anxiety / depression or other psychosocial issues?
- U – Does the patient have Hunner’s ulcers (now known as lesions)
- T – Does the patient have tight or dysfunctional pelvic floor muscles.
They tested this system with 239 men and women. The incidence of domains was Infection 11%, Neurologic/Systemic 51%, Psychosocial 81%, Ulcers 18% and Tenderness 85%. Patients had, on average, 2.46 domains and 65% had 2 or 3 positive domains. Only 5% had none. The greater the number of domains, the great the symptoms. Hunners lesions increased symptom scores. The conclude that the INPUT system replicates the validity and clinical utility of the UPOINT system. They also believe that patients may benefit from multimodal therapy up front for each extra domain rather than relying on the sequential tiered approach found in the AUA Guidelines.
Author – Jill Osborne MA
Created – January 16, 2017
Updated:January 31, 2023