As if having one chronic pain condition wasn’t enough, some IC patients are more likely to be diagnosed with others, including fibromyalgia. Five years ago, I joined the rank of IC patients diagnosed with fibromyalgia during a particularly stressful time in my life. Once I was diagnosed, I was able to look back and see different times throughout my life when I showed signs of fibromyalgia but was instead treated for just one specific area of pain at a time. I had shots in my shoulders, therapy for my back, a regimen for foot pain and on the list goes. Suddenly it all made sense as I realized “normal” people don’t wake up with pain somewhere every single day.
While I’d spent my life learning to live with bladder pain and pressure, fibromyalgia was a whole new adjustment and challenge. Unfortunately, I’m not alone. Many patients find that fibromyalgia and IC go hand-in-hand. Sometimes IC comes first; sometimes fibromyalgia comes first. But no matter what, understanding the symptoms and treatments is important for all IC patients to be able to better identify any additional changes that might occur in their bodies.
Symptoms
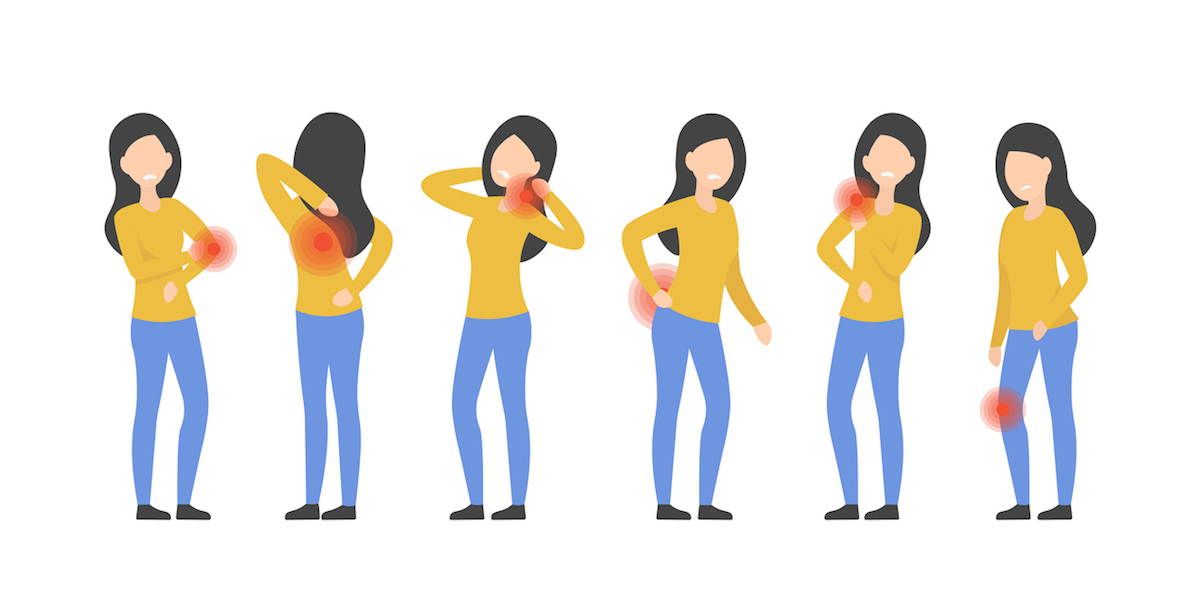
One of the most common perceptions of fibromyalgia is pain throughout the body. My family physician told me that something like banging into a table might smart for a “normal” person but would be very painful for someone with fibromyalgia. Though that isn’t incorrect, it doesn’t paint a full picture of what the condition actually feels like. Fibromyalgia has three main symptoms: widespread pain, fatigue and cognitive difficulties.1
Widespread pain is defined as pain that has lasted for three months and occurs in both sides of your body as well as above and below the waist.1 The pain can be a dull ache, a sharp pain or even a burning sensation. Overall, people with fibromyalgia can be more sensitive to pain than those without fibromyalgia, which is referred to as abnormal pain perception processing.2
Fatigue, another main symptom of fibromyalgia, is so pronounced in fibromyalgia patients that sometimes Chronic Fatigue Syndrome and fibromyalgia are used interchangeably. No matter how long they’ve slept, fibromyalgia patients usually wake up tired. Their sleep is disrupted by pain and other sleep disorders that can go along with the con-dition.1 Add in an IC bladder waking them up throughout the night for the restroom and it’s a perfect storm for fatigue.
The third main symptom is cognitive difficulty, also known as “fibro fog.” Patients may notice that it is harder to focus or pay attention to mental tasks.1 Something simple, like remembering the name of an object, can be difficult, especially during times of flares.
Fibromyalgia also has other symptoms that are common amongst patients, including: stiffness, depression, anxiety and headaches (includ- ing migraines).2 Some patients describe the pain as feeling like you are bruised throughout your body. And many of us have pain that rotates throughout our bodies. WhileI have some areas of my body that always hurt, I usually have random other pain that will show up in dif- ferent parts of my body most days. I never know what is going to be affected from one day to the next from my knees to my toes to my elbows to my neck.
Risk Factors
Fibromyalgia affects about 4 million (2%) adults in the United States.2 While an IC diagnosis has been shown to have a higher risk of developing fibromyalgia, other risk factors contribute as well. Women are more likely than men to be diagnosed.1 Genetics can play a role. If you have a direct family member with fibromyalgia, you are more likely to have the condition as well.1
Age can also play a role. Patients are diagnosed at a variety of ages but most are diagnosed in middle age with the risk increasing the older you get.2 Highly stressful or traumatic events make people more likely to develop fibromyalgia.2 (My diagnosis fits right into this category since it happened at age 36 in the midst of an incredibly stressful time.) Repetitive injuries, obesity and some viral infections can also put people at higher risk for developing fibromyal- gia.2
Diagnosis
Fibromyalgia has no definitive test for diagnosis. It is diagnosed by symptoms and their longevity. Finding the right doctor can require some research. Don’t be surprised if you visit two or three until you find a doctor you can work with. Primary care physicians are the first to suspect fibromyalgia and can often recommend and refer you to a good medical provider in your area. The types of doctors who are most likely to be familiar with fibromyalgia are rheumatologists, neurologists and pain management doctors.3
If the doctor you see suspects you have fibromyalgia, he or she may do an exam to determine if you are tender in a certain number of specific spots on your body before diagnosing fibromyalgia.4 A physical exam can also help the doctor determine whether there is a different underly- ing cause for your pain. You may have to have a few tests before officially getting the diagnosis.4
The three general criteria currently recommended for diagnosing fibromyalgia are pain and other related symptoms (fatigue and cognitive problems), symptoms that last at least three months at the same level and the absence of any other health problem that would explain the pain and symptoms.4
Treatment
Three drugs have been approved in the United States for treating fibromyalgia: duloxetine (Cymbalta), milnacipran (Savella) and pregabalin (Lyrica).4 Both Cymbalta and Savella change the brain chemicals that help control pain levels. Lyrica works by targeting the nerve cells involved in pain transmission and keeping them from being overactive. Another pre- scription medication, gabapentin (Neurontin), is not specifically FDA- approved for treating fibromyalgia but works the same as Lyrica.4
While pain medication and anti- inflammatory drugs do not usually work well for fibromyalgia pain, they can work to alleviate other issues (like arthritis) that are contributing to and/or aggravating the pain.4
Patients have found self-help treatments to be important in living a better quality of life. While moving a body that is painful may seem coun- terintuitive, movement and gentle exercising can help alleviate or lessen some fibromyalgia pain. Exercises like walking, water activities (swimming or aerobics) and biking can work when done gradually. Physical therapists can help patients with learning stretches and even exercise regiments that can help reduce pain and improve physical health.1 I can tell a significant difference in my pain levels on days I do and don’t do stretches. The yoga-like stretches I’ve learned through physical therapy through the years really do help.
Other issues that can exacerbate fibromyalgia pain are stress and lack of good sleep.1 Anything patients can do to reduce and manage stress can help with their pain. The same is true for sleep. Good sleep can certainly be an issue for fibromyalgia and IC patients. Setting a good routine and even building in short naps on rough days can be very helpful.
Learning to pace yourself is essential. If you wake up and are having a good day, don’t clean your house from top to bottom and send your- self into a flare that can last for days or weeks. Instead, take things easy and spaced out so as not to overdo it.
Finally, supportive family members, friends and other patients make dealing with any health issue easier. Connect with other patients dealing with both fibromyalgia and IC on the IC Network’s Patient Forum for additional support.
The “IC’s Related Conditions” series takes a look at conditions that can go hand-in-hand with IC. Not all patients have all of these conditions, but IC patients are more prone to be diagnosed with these conditions than the general population. (As always, this is not intended as medical advice and is for informational purposes only. Any and all medical questions should be addressed with your doctor.)
References
- Mayo Clinic Staff. Fibromyalgia. MayoClinic.com. Aug. 11, 2017.
- Centers for Disease Control and Prevention. Fibromyalgia. Last reviewed Jan. 26, 2020.
- Kowlowitz E. Who Treats Fibromyagia? Spine Universe. Last updated March 15, 2019.
- Amigues I. Fibromyalgia. American College of Rheumatology. Last updated March 2019.