Pain Management for Interstitial Cystitis
While pain is not always a symptom in IC, for the men and women who have it, it can be agonizing, as if razors are cutting our bladders. Yet, for years, patients have been told that it’s all in their heads and that they just need to ignore the pain. Hogwash!! Would you deny a cancer patient pain care?? Of course not. IC pain has been rated equivalent to cancer pain and deserves urgent, compassionate treatment. Each patient faces three challenges: (1) To isolate where the pain is coming from, (2) to catch pain early and (3) to use a balance of self-help and traditional treatments to control and reduce pain.
- Introduction
- Potential Sources of Pain
- Working With Your MD
- Pain Care Principles
- Treatments Options – Medications
- Treatment Options – Procedures
- Treatment Options – Complementary & Alternative
- Additional Resources & Helpful OTC Products
Introduction
Who would have thought that the bladder could hurt so badly as to drive a patient to complete despair. We associate pain with broken arms, legs, appendicitis, or childbirth, not our bladders. Yet, the pain experienced by many interstitial cystitis patients has been rated equivalent to that experienced by cancer patients and can be agonizing.
As an IC pain patient, I can relate. In the year that my symptoms began, I struggled to sleep more than an hour at a time, was unable to drive in a car without searing pain and found many basic daily activities difficult, if not impossible. There were moments when the pain was so severe that I felt as if I was dying. Yet, as I write this today, I can honestly share with you that I found relief for my pain and a dramatic improvement in my symptoms.
Fighting pain requires building a solid foundation of knowledge, discipline and skills. You, the IC patient, must take the time to gather information on pain management. You must be open and willing to try various IC & pain treatments as you work with your physician. Although many of you love coffee (regular & decaf), tea (regular & green) and soda, you must be disciplined enough to stop those things which we know badly irritate the bladder. A hot cup of peppermint tea, chamomile tea or steamed milk is much more bladder friendly.
Pain also takes a toll on our spirit, emotions and family lives. I want to remind you that you have done nothing wrong nor do you deserve to be alone. When you can’t travel comfortably, invite family and friends over to your house for a potluck or video night. When you’re feeling confused about your IC, come check the ICN web site for new articles. If you need support, you can visit our ICN Support Forum 24 hours a day for new ideas and encouragement. You are not alone! – Jill Osborne, ICN President & Founder
Bladder Pain Is Real 
The bladder, like any other part of the body, can generate pain so severe that patients require immediate medical care and treatment. Unfortunately, IC patients struggle to overcome the perception their bladder pain “isn’t that bad”or is very mild in nature. The first published epidemiological study on IC in 1987 found that the pain of IC rated equivalent to that of cancer pain on the McGill Pain Scale. Similarly, the quality of life for some IC patients was rated equivalent to patients in end-stage renal failure. Given the fact that patients suffering from cancer pain or kidney failure usually receive immediate care and attention, many IC patients also deserve prompt and compassionate pain care.
Potential Sources of Pain
IC pain can originate not only from the bladder but also from nearby muscles, nerves and even referred pain from other parts of the body. With time, most patients learn the subtle difference in symptoms between an IC flare caused by direct bladder irritation (i.e. diet) versus a muscle spasm (i.e. sex, driving in a car,etc.). Bladder wall irritation has a tendency to create more of a sharp, intense pain. Pelvic floor muscle spasms create a deeper, heavier burning sensation that can make sitting more uncomfortable. Nerve pain can be more electrical, hot or searing in nature. Each potential source of pain has its own symptoms and treatments.
1. The Bladder Wall (AKA urothelium):
 The urothelium is the most specialized epithelium in the human body and all of mammals. It must act as a permeability barrier to protect underlying tissues from urine while also stretching as the bladder fills with urine. When it is damaged, urine can reach into the deeper layers of the bladder wall where it will trigger irritation and/or inflammation. Bladder wall irritation may provoke frequency, pressure and/or pain. Some patients may just have frequency, particularly at night, while others may experience pain as the dominant symptom.
The urothelium is the most specialized epithelium in the human body and all of mammals. It must act as a permeability barrier to protect underlying tissues from urine while also stretching as the bladder fills with urine. When it is damaged, urine can reach into the deeper layers of the bladder wall where it will trigger irritation and/or inflammation. Bladder wall irritation may provoke frequency, pressure and/or pain. Some patients may just have frequency, particularly at night, while others may experience pain as the dominant symptom.
Potential Pain Triggers For Bladder Wall Irritation:
DIET – The most common trigger is diet. Most patients report intense discomfort and/or pain after eating or drinking certain foods, particularly coffees, sodas, various teas, fruit juices (citrus, cranberry juices) and tomato products (i.e. tomato soup, juice, pasta sauce, etc.). Thus, diet modification and avoiding those foods known to irritate the bladder is the easiest and, often, most effective way of reducing bladder wall discomfort.
HORMONES – Menopause and hormones also influence the bladder wall and vulva. As estrogen levels drop, the tissues of the vulva, urethra and bladder become thinner, more vulnerable and sensitive to stimulation. Most care providers will test hormone levels in patients struggling with pain and discomfort and, if needed, suggest an estradiol vaginal ring (aka Estring), hormone replacement therapy or a compounded, preservative-free estrogen cream.
CHEMICALS – From chlorine in swimming pools to perfumed laundry products, IC patients have long known that certain chemicals provoke urethral, bladder and vaginal discomfort. Many brand name laundry detergents (i.e. Cheer, Tide), bubble baths and soaps (i.e. Irish Spring, Dial, etc.) are known to trigger urethral irritation and pain. Similarly, the heavy chlorine found in swimming pools and hot tubs can be harsh irritants. Even bath soaps, particularly liquid soaps that are heavily perfumed, can trigger an IC or vulvodynia flare.Dove soap for personal hygiene and Ivory Snow or Dreft for the laundry are better tolerated by IC patients. Fabric softeners or other products that add a scent to clothes should also be avoided.
SMOKING – Unsurprisingly, smoking is the number one cause of bladder cancer. As the body excretes the thousands of harmful chemicals found in smoke, they become concentrated in urine and can cause irreversible damage to the bladder. Research released by the University of Florida in 2006 also confirmed that these chemicals actually reduce the ability of the body to heal itself. As such, smoking can badly irritate an IC bladder. Patients are urged to stop smoking or, at a minimum, try the nicotine patch.
2. Bladder Spasms
Bladder spasms occur when the muscles in the bladder contract suddenly and unexpectedly. Men and women may experience a “flip-flopping” sensation in their bladder. For some women it can be a deeper sensation in the vagina, very similar to the irritation felt with a yeast infection. Still others may have brief but excruciating pain at the end of urination when their bladder walls briefly touch.
Potential Triggers For Bladder Spasms: Catheterizations, diet-induced bladder irritation, UTI, etc.
3. Pelvic Floor Muscles
The pelvic floor muscles provide support for the organs in the pelvis including the bladder and uterus. Over the past 20 years, urologists and gynecologists evaluating IC patients have often found pelvic floor muscles that are tender to touch and resemble tight rubber bands. Pelvic floor tension often occurs as a result of pain in the bladder, prostate, rectum and vagina. If pain persists, muscle tension can become habitual to the point that the muscles become shortened and distorted. Patients may subconsciously tighten muscles in a guarding reflex to help prevent further pain. In both cases, trigger points can also develop.
Most IC clinicians now assess for pelvic floor dysfunction and have physical therapists on staff to treat pelvic floor muscle tension. Ignoring the musculature and/or only treating the bladder, can extend pain for a much longer period of time. Ideally, both the pelvic floor muscles and bladder are treated at the same time.
The classic symptom of a tight pelvic floor is difficulty in starting urination. Patients usually have to wait a few seconds (or longer) for their pelvic floor to relax enough to urinate. Patients may feel is as if there is a foreign object in the vagina or rectum. Other patients report a deeper burning sensation that can feel like a vaginal or yeast infection.
Potential Triggers For Pelvic Floor Muscle Discomfort: Sexual intercourse, driving, sitting for long periods of time, traveling and aggressive or jarring exercise (i.e. running or Stairmaster). Of course, anything that irritates the bladder wall and provokes pain can also trigger pelvic floor tension.
4. Neuropathic Pain
 Neuropathic pain results from trauma or damage to a nerve and is usually experienced as chronic pain. In IC, this is often shown through reduced bladder capacity when the nerves in the bladder provide the sensation that it is painfully full, even with a small amount of urine.The normal threshold of stimulation can be reduced to the point where pain results from irritants that wouldn’t usually cause pain (i.e. a small amount of urine). Nerves can also become too responsive (aka hyperalgesia). In this situation, the patient may feel prolonged, exaggerated pain and discomfort.
Neuropathic pain results from trauma or damage to a nerve and is usually experienced as chronic pain. In IC, this is often shown through reduced bladder capacity when the nerves in the bladder provide the sensation that it is painfully full, even with a small amount of urine.The normal threshold of stimulation can be reduced to the point where pain results from irritants that wouldn’t usually cause pain (i.e. a small amount of urine). Nerves can also become too responsive (aka hyperalgesia). In this situation, the patient may feel prolonged, exaggerated pain and discomfort.
Neuropathic pain can also affect nearby tissues and make them more sensitive to touch (i.e. the vulva and penis) in a condition called allodynia. Some women may struggle with a sensation of vulvar discomfort and/or vulvodynia, while men may experience rectal or penile pain. In some cases, sensitization can affect the pudendal nerve, creating a painful arousal sensation of the clitoris that can last for hours or longer. Both of these conditions usually resolve with time as inflammation decreases.
Similarly, nearby organs may also trigger pain in the bladder. Research conducted at the University of Pittsburgh found significant bowel-bladder cross-sensitization within the afferent “pain” nerve fibers in the pelvis. When the bowel is irritated,“the very nerves that carry signals for uncomfortable bladder sensation had become hypersensitive or overly sensitive.” This could explain why so many IC patients also struggle with bowel discomfort and Irritable Bowel Syndrome (IBS) in addition to their IC and vice versa.
Neuropathic pain is felt as a sharp, electrical or a chronic burning sensation. There may be an increased sensitivity to touch in the general area or a lack of sensation.
Potential Triggers For Neuropathic Pain: Diabetes, accident, injury, long-term chronic pain.
5. Urethral Pain
Many patients struggle with pain in their urethra and may have been diagnosed with urethral syndrome or urethritis prior to their diagnosis of IC. For both men and women, urethral discomfort may be the result of spasm of the urethra or a urethral stricture. Some soaps, spermicides, lubricants and/or detergents can also trigger irritation in the urethra. Similarly, catheterization is well known to create short-term urethral pain, particularly the first few times a patient urinates afterwards. Bladder infections are also notorious for causing urethral sensitivity and often trigger a sensation of burning during urination. Some women may also have an infection of the paraurethral glands,a small sponge like gland that wraps around the urethra about half way up towards the bladder. Patients with this type of infection often experience intense discomfort at the moment of penetration during sexual intercourse.
Urethral pain is usually felt as a burning sensation during or after urination. Most patients experience a sharp, burning pain with the first few voids after catheterization that quickly resolves.
Potential Triggers For Urethral Pain: Infection, chemical irritants (soaps, laundry detergents, spermicides, chlorine from pools or hot tubs), catheterization.
6. Referred Pain From Other Sources
Patients who don’t respond to any traditional IC therapies need to take the time to rule out other potential conditions, such as: pudendal nerve entrapment, endometriosis, fibroids, ovarian cysts, bladder cancer and low back injuries.
Working With Your MD
Finding a Medical Care Provider
Most patients rely on their urologist or primary care provider to provide pain care. However, there are many physicians who are uncomfortable or unwilling to provide prescriptions for pain medications. They may refer their patients to a pain specialist and/or clinic instead. Pain specialists are often anesthesiologists who have received training in managing complex, intractable pain.
When looking for a pain specialist, talk with other patients and/or support group leaders. Ask them who they feel is the most compassionate and educated in treating pain. Many organizations can also provide referrals. Many of their web sites also have searchable member lists, including:
- International Pelvic Pain Society
- American Academy of Pain Medicine
- American Academy of Pain Management
- American Board of Pain Medicine
- American Medical Association
Be Willing to Talk About YOUR Pain
 When you visit a pain clinic, be prepared to talk about your pain in depth. Saying “I’m in pain” doesn’t provide enough information. You’ll need to share where it’s located, what it feels like, when it occurs and how it changes throughout the day. It’s also important to remember that the physician may have never experienced IC or bladder pain and may not understand what you are going through. Try being more descriptive. Share how your bladder pain limits your life. Does it prevent you from sleeping, from working, from shopping? Often, when you describe your limitations, doctors get a much better grasp of how serious it actually is.
When you visit a pain clinic, be prepared to talk about your pain in depth. Saying “I’m in pain” doesn’t provide enough information. You’ll need to share where it’s located, what it feels like, when it occurs and how it changes throughout the day. It’s also important to remember that the physician may have never experienced IC or bladder pain and may not understand what you are going through. Try being more descriptive. Share how your bladder pain limits your life. Does it prevent you from sleeping, from working, from shopping? Often, when you describe your limitations, doctors get a much better grasp of how serious it actually is.
One mistake is to demand pain medication. This may make you look like a “drug seeker”or “doctor shopper.” It’s much better to approach physicians by asking how you can work together to improve your quality of life and ability to function.
Pain Care Principles
Catch Pain Before It Gets Out of Control
Imagine this scenario. An IC patient calls her doctor crying in pain. When the doctor asks, “How long have you had this?” The patient says, “Two months.” The doctor asks,“Why didn’t you come in earlier?” The patient says, “I hate using prescriptions… I just thought I’d bear it. That’s what I do.”
Fighting pain is like fighting a fire. The smaller it is, the less intervention it may take to resolve. When pain is ignored it can become more intense and difficult to treat as more tissues (and/or nerves) become irritated. Catching pain early is vital! Patients who delay seeking help or using medication until “the pain gets real bad” may suffer needlessly.
Combination Therapy is Essential
Every good IC management program includes a combination of medication, self-help and/or interventional strategies that can help. Thus an IC patient may be using some prescription medication to soothe her bladder. If she has pelvic floor dysfunction, she may visit the physical therapist once a week. To help reduce stress and anxiety, she may also take a class on stress management and/or find someone to talk with. On a daily basis, she is also avoiding foods that can trigger bladder pain and discomfort, such as coffees, teas, fruit juices and sodas. She walks to exercise and, before bedtime, listens to a guided relaxation tape to help relax her muscles.
Treatments Options – Medications
When considering various pain therapies, please talk with your physician about the pros and cons of each treatment you are considering. All medications and supplements come with the risk of side effects and should be used appropriately. Some drugs may cause serious side effects if they are combined with other medications. Even over-the-counter and herbal medications can trigger serious reactions when combined with others.
Anticholinergics
Anticholinergic medications, such as Ditropan and Detrol, slow down bladder overactivity and may be helpful for patients struggling with an overactive bladder and/or bladder spasms. These are NOT pain medications. Potential side effects include constipation, dry mouth and lethargy.
Antidepressants
Many patients are offended that a doctor would recommend a “psychiatric” medication, implying that they don’t believe the pain is real. Happily, this is not the case. Antidepressants have long been useful in the treatment of long-term chronic pain and appear to strengthen the body’s internal pain fighting mechanism. Antidepressants can also improve the quality of sleep and may increase the effectiveness of other pain medications.
Two forms of antidepressants are currently available: (1) tri-cyclic antidepressants (TCA’s), including amitriptyline(Elavil®), desipramine (Norpramin®), imipramine (Tofranil®) and nortriptyline (Aventyl®, Pamelor®) and (2) Selective Serotonin Reuptake Inhibitors (SSRI’s), including citalpram, escitalopram (Lexapro), fluoxetine (Prozac®),fluvoxamine (Luvox®), paroxetine (Paxil®) and sertraline (Zoloft®).
They, unfortunately, do come with a host of side effects including: drowsiness, dry mouth, weight gain, blurred vision, impaired thinking, tiredness, worsening of glaucoma, constipation and more. For some patients, they may cause a pounding heart, tachycardia or arrythmia that may preclude their use. If a patient experiences an irregular, rapid or pounding heartbeat, they should notify their physician immediately. The dosage may need to be reduced or medication stopped completely.
Antihistamines
Antihistamines can play an important role in the treatment of IC discomfort. Antihistamines help reduce histamine induced irritation in the bladder, particularly in patients with a history of allergies. They may also dramatically improve sleep quality and anxiety. When used with opioids, antihistamines apparently help to increase the pain reducing action of the opioid. Side effects may include an increase in intense dreaming, sedation and dry mouth. Patients sensitive to chemical fillers and preservatives may find that hydroxyzine pamoate (Vistaril®) is easier to tolerate thanhydroxyzine HCL (Atarax®).
Anti-seizure Medications
First used to prevent seizures, anticonvulsants have also been found to help some pain disorders.Carbemazepine (Carbatrol®, Tegretol®) is FDA approved to treat trigeminal neuralgia. Gabapentin (Neurontin®) is approved for use with postherpetic neuralgia and appears to be effective for people struggling with neuropathic pain.Topiramate (Topamax®) has been used to prevent migraines as well as neuropathic pain. Clonazepam(Klonopin®), valproic acid (Deparkote®) and phenytoin (Dilantin®) may also have some pain reducing effects. Side effects for this class of medications can be profound, including decreased mental alertness, dizziness, drowsiness and, in the case of toprimate, the development of glaucoma.They should be monitored carefully.
Hybrid Prescription Pain Medications
Tramadol (Ultram®) and tramadol with acetaminophen (Ultracet™) are prescription pain medications used for moderate pain. It is a weak opioid that acts on parts of the brain and spinal cord to reduce pain sensation. It also appears to reduce the size of the pain signal. Propoxyphene (Darvon®, Darvocet®) is a mild opioid analgesic related to methadone and is used for mild to moderate pain.
Muscle Relaxants
Muscle relaxants can be helpful for patients struggling with pelvic floor tension. While known for their treatment of anxiety, diazepam (Valium®) and cyclobenzaprine (Flexeril®) have been found to be helpful in the treatment of muscle spasms. Side effects include fatigue and depression.
Opiates
Opioids, also known as narcotics, are the mainstream of treatment for moderate to severe pain. They are used when other therapies are not helpful in reducing pain and may be discontinued once other treatments help reduce overall pain levels.The side effects of opioids may include constipation, nausea, vomiting, itching, respiratory depression, edema, confusion and urinary retention. For IC patients, constipation can antagonize already sensitive bladders, thus patients using these medications may need to use a stool softener or soluble fiber, such as Heathers Tummy Fiber!
To determine who should use an opioid, physicians may look at several factors, including the intensity of pain, age, other medications, other illnesses and response to other pain therapies. If, for example, a patient is taking other medications that cause respiratory depression, her physician may not wish to use opioids.
IC patients with intermittent pain due to flares may have a prescription of a short acting opioid (i.e. codeine, hydrocodone) on hand for use on an “as needed” basis. Persistent pain patients will often be prescribed a longer acting sustained release opioid (i.e. morphine, hydromorphine) that can fight pain on an hourly basis. Patients with breakthrough pain may utilize a variety of medications as discussed with their physician.
Opioid prescriptions can bring up a wide variety of issues for patients and physicians, including: appropriate vs . inappropriate use, drug abuse, addiction, dependency and tolerance. An appropriate use of pain medications is to promote functionality in a patient’s life and to provide comfort from symptoms so that she can return to work and fulfill her daily responsibilities. In contrast, a patient taking drugs to escape life’s problems or taking more than prescribed or purposely “getting high” is using the drugs inappropriately.
Research has demonstrated that fewer than one in 100 patients using opioids for pain management develop an addiction. Patients can, however, develop a physical dependence or tolerance to the medication. This is not addiction. In physical dependence, the body has adapted to the presence of pain medication after continued use.Thus, when the medications are stopped, they can develop withdrawal symptoms. This can be avoided by gradually reducing the dose of the medication over time. Tolerance occurs when, after long-term use of a drug, an increased dosage is needed to produce the same effect.
Opioids may be available as oral medications, rectal suppositories, transdermal patches, subcutaneous injections, intravenous injections or by epidural, subdermal and intramuscular injections. They are grouped by their strength and/or duration of action (short half-life drugs or long-acting sustained-release agents). Patients using any of these medications should review and discuss their dosages and/or dosing schedule with their personal careproviders. Dosages will vary depending upon the form of the medication. Patients should never self medicate and/or increase a dosage without first talking with their doctors.
Opioids Used For Moderate Pain:
- codeine
- hydrocodone (i.e. Lortab, Vicodin),
- oxycodone (i.e. Oxycontin, Percocet)
Opioids Used For Severe Pain:
- meperidine (i.e. Demerol)
- hydromorphone (i.e. Dilaudid)
- methadone (i.e. Dolophine)
- fentanyl (i.e. Duragesic, Actiq)
Opioids Used For Extended Use (i.e. Time Release):
- Long acting morphine (i.e. MS Contin)
- Long acting oxycodone (i.e. Oxycontin)
- methadone (i.e. Dolophine)
- fentanyl (i.e. Duragesic)
Urinary Anesthetics & Analgesics
 Oral phenazopyridine hydrochloride (Azo Standard-OTC or Pyridium®) is a urinary anesthetic. It is best known for turning urine orange in color and may be helpful for mild discomfort. Patients may find, however, that it has little effect on moderate to severe pain. This medication is not recommended for long-term use because of its potential to affect the production of blood cells.Urised® is a “combination” medication that contains an anesthetic and an anticholinergic agent that helps to relax the bladder.
Oral phenazopyridine hydrochloride (Azo Standard-OTC or Pyridium®) is a urinary anesthetic. It is best known for turning urine orange in color and may be helpful for mild discomfort. Patients may find, however, that it has little effect on moderate to severe pain. This medication is not recommended for long-term use because of its potential to affect the production of blood cells.Urised® is a “combination” medication that contains an anesthetic and an anticholinergic agent that helps to relax the bladder.
Treatment Options – Procedures
Rescue Instillations
In recent years, rescue instillations, aka anesthetic cocktails, have become popular. Usually consisting of a solution of a local anesthetic (intravesical lidocaine and/or marcaine), an alkalinizing agent (sodium bicarbonate) and a bladder coating (Elmiron® or heparin), it is placed directly into the bladder for an instant numbing effect. Many physicians have created their own customized solutions and treatment schedule.
In general, rescue instillations are used up to three times a week for two or three weeks and then reduced to a weekly, monthly and/or on “as needed” basis. Anesthetic cocktails can also be useful in the diagnosis of IC. If a patient has a strong symptom relief from the solution, it implies that the origin of the pain is the bladder. Safety notice
Some patients are taught to administer these instillations at home. It is critically important for the patient to follow the instructions and dosages of the ingredients exactly as determined by their physician. Under no circumstance should a patient adjust the formula their own. Lidocaine, if used improperly at high dosages, can result in a serious complications and/or death.
Electrical Nerve Stimulation
With transcutaneous electrical nerve stimulation (TENS), mild electric pulses enter the body. This lasts for anywhere from minutes to hours and is done two or more times a day. The leads are either placed on the lower back or just above the pubic area, between the navel and the pubic hair. Although scientists do not know exactly how TENS relieves pelvic pain, it has been suggested that the electrical pulses may increase blood flow to the bladder, strengthen pelvic muscles that help control the bladder and/or trigger the release of substances that block pain. TENS is relatively inexpensive and allows the patient to take an active part in treatment. It does, however, require a prescription and training to use. TENS units are available for purchase at most medical equipment companies and should cost less than $100.
Nerve Blocks
Nerve blocks can be helpful when pain is localized and unresponsive to other pain therapies. When a nerve is blocked by injecting a numbing agent, it may provide pain relief for a limited period of time. These can be helpful for patients who struggle with clitoral pain and/or a painful arousal sensation as part of their IC symptoms. These are usually performed by a pain specialist, rarely require hospitalization and may be repeated.
Pain Pumps
A pain pump allows pain medication to be slowly delivered into the blood stream or spinal cord. Ideal for patients recovering from surgery, pain pumps provide scheduled, safe dosages of medication over a longer period of time via a small computer. Pain pumps do come with some risk, including the development of infection. Pain pumps are carefully supervised by pain management specialists and/or anesthesiologists.
Trigger Point Injections
Patients struggling with painful trigger points may respond well to an injection of lidocaine directly into the trigger point so that it can be manipulated without further pain and discomfort. This may be recommended by a physical therapist but is performed by a gynecologist or urologist.
Treatment Options – Complementary & Alternative
BIOFEEDBACK
Biofeedback has been used for many years for pelvic floor disorders and incontinence. Through the use of small sensors which signal when muscles are tense, patients are taught to consciously relax the muscles and thus reduce that discomfort. Its long-term success, however, depends upon the patients’ willingness to use the techniques and their commitment to build their relaxation skills. Luckily, this is often covered by health insurance and is usually obtained through a physical therapist.
EXERCISE
Because movement often makes the pain feel worse, most patients tend to “brace” or “guard” their muscles against pain. Unfortunately, this guarding behavior often can create long-term discomfort. Normal movement must be restored to the area. Gentle movement and exercise is the key to increasing mobility, flexibility and functionality. For the IC patient, the goal is to choose exercises that are not jarring to the bladder and pelvis, such as walking, swimming and some forms of yoga. By improving blood and oxygen flow to muscles throughout the body, it will improve the patient’s sense of well-being, reduce stress and improve sleep quality.
Fair warning. If a movement hurts, such as using a stair stepper or jogging, patients should temporarily suspend that activity in favor of something gentler to the body. The goal is to soothe the bladder and calm the nerves to give them time to recover. If a patient persists in doing an activity that is causing pain, it defeats the purpose. Patients who want to burn calories and/or do aerobic activities can benefit from using a rowing machine or elliptical at the gym.
Heat & Cold Therapy
While some patients find that the use of heat and heat packs can be comforting, others do well with cold packs. Heat helps to calm aching muscles, reduce spasms and increase circulation. A variety of heating pads are available for IC patients, developed specifically to sit over the bladder that are available for purchase in the ICN Shop.
Microwaveable pads are usually filled with rice, flaxseed and/or other natural materials. They will hold heat for 15 to 30 minutes, depending upon their size and shape. (Many can also be placed in the freezer and used as a cold pack.)
 Electric heating pads are commonly used to provide steady, high heat. To prevent burns, an electrical heating pad should never be used during sleep. Electrical heating pads that come with an automatic turn-off switch are best because they help avoid potential fire and/or burns.
Electric heating pads are commonly used to provide steady, high heat. To prevent burns, an electrical heating pad should never be used during sleep. Electrical heating pads that come with an automatic turn-off switch are best because they help avoid potential fire and/or burns.
Bodiheat one-time use heating pads are a popular favorite for patients with bladder pain because they can be placed directly on underwear or pajamas and worn for an entire day or night, such as during work, while driving, etc.
Additional Resources
Other Organizations
- American Chronic Pain Assn, P.O. Box 850, Rocklin, CA 95677, (916)632-3280
- American Pain Society, 4700 W. Lake Avenue, Glenview, IL 60025, (708)375-4715
- International Assn. of the Study of Pain, 9090 NE 43rd St., #306, Seattle, WA 98105, (206)547-6409
- American Academy of Pain Management, 139747 Mono Way, Suite 1, Sonora, CA 95370, (209)533-9744
- American Academy of Pain Medicine, 4700 W. Lake Avenue, Glenview, IL 60025, (708)375-4731
- American Society of Addiction Medicine 4601 North Park Ave, Arcade Suite 101 Chevy Chase, M.D. 20815, Telephone 301/656-3920
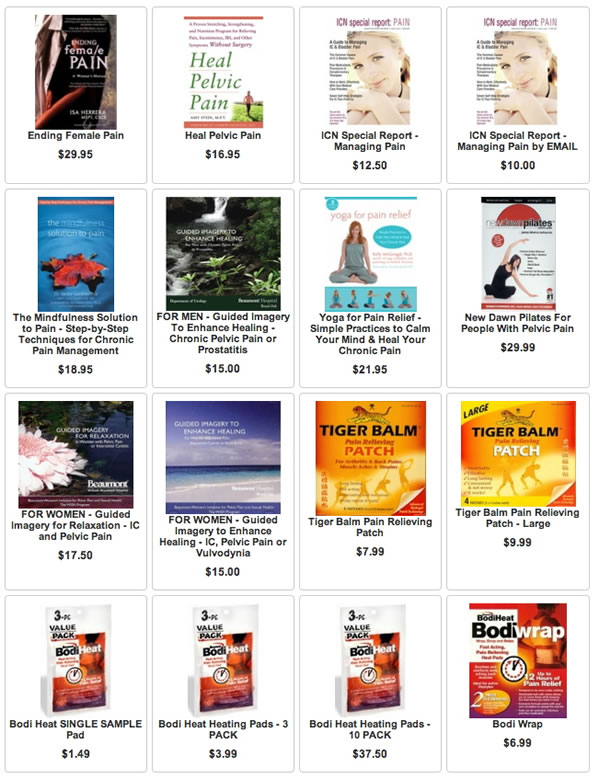
Helpful Products
Author: Jill Osborne, MA
Created: Revised July 6, 2022
Full references and a much larger discussion on pain care, are available in the ICN Special Report: Pain Mgt..