Eosinophilic Cystitis
Welcome to the ICN’s Eosinophilic Cystitis Resource Center. Launched in 1999 as the first on-line resource center for EC patients, we’re happy to share that there are new resources and studies available that provide hope to patients struggling with this rare form of cystitis.
What is Eosinophilic Cystitis
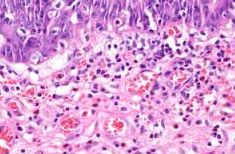 Eosinophilic cystitis (EC) is a rare bladder disorder characterized by the build up of eosinophils (a type of white blood cell) in the bladder.(1) Eosinophils normally live in the blood stream in small quantities. The body will produce more in response to allergies, skin conditions, infections, autoimmune diseases, some cancers and bone marrow disorders. In some conditions, however, eosinophils build up in various organs and tissues where they can cause injury and inflammation, including: the bladder, esophagus, stomach, colon, blood vessels.(2)
Eosinophilic cystitis (EC) is a rare bladder disorder characterized by the build up of eosinophils (a type of white blood cell) in the bladder.(1) Eosinophils normally live in the blood stream in small quantities. The body will produce more in response to allergies, skin conditions, infections, autoimmune diseases, some cancers and bone marrow disorders. In some conditions, however, eosinophils build up in various organs and tissues where they can cause injury and inflammation, including: the bladder, esophagus, stomach, colon, blood vessels.(2)
In most cases, the cause of eosinophilic cystitis is unknown though it can be a symptom of hypereosinophilic syndrome.(3) Eosinophilic cystitis has mimicked bladder tumor and cancer in many published case reports due to the formation of tumor like structures that, in fact, are composed of eosinophils. Researchers in India recently shared a case study of a 16 year old male who was discovered to have a mass in the bladder with swelling. Upon biopsy, it revealed eosinophils rather than cancer.(4)
Eosinophilic cystitis was also associated with eosinophilic cholecystitis in the case of a 30 year old patient who was treated for gallstones and had a biopsy due to bladder symptoms. Both conditions were associated with eosinophil proliferation. (5)
EC has also been associated with the use of various medicines and, in one published study, a chinese herb. Researchers in Japan shared the story of a 19 year old woman with bladder symptoms after she began using an herb named “Seijoh-bohhuh-toh.” Lymphocyte stimulation tests with the herb were positive and her symptoms resolved after she stopped using it.(6)
EC has occurred in men and women of all ages, including children as young as three years old.(7,8,9,10) Numerous case reports are available at the National Library of Medicine.
Symptoms of EC
- Painful urination
- Blood in the urine (hematuria)
- Urinary frequency
- Pelvic pain
Diagnostic Methods
Like interstitial cystitis (IC), patients with EC may wait years before receiving a correct diagnosis. The diagnosis begins with a full patient history and physical examination. Urinalysis may reveal blood and, in some cases, eosinophils in the urine. An ultrasound should also be performed which may show thickening (or a mass) in the bladder. The gold standard test is biopsy of the bladder wall, which should show high eosinophils invading the bladder wall as well as chronic inflammation.
Allergy testing is often useful in those patients with a history of allergic diseases (i.e. hay fever, asthma) to identify any allergens.
Treatments
For patients who have a known trigger, the cure can be as simple as eliminating or controlling that cause. If not, the use of high, tapering doses of corticosteroids, anti-inflammatories and antihistamines are suggested.
Montelukast sodium (i.e. Singulair) has been found to be successful in an EC patient who also suffered from asthma. She received montelukast daily for four weeks and went into a complete remission. (11)
Another medication used to treat allergies, suplatast tosilate, was found helpful in the treatment of EC in a 49 year old man in Japan. After the discovery of severe EC and bladder wall thickening, he was treated initially with prednisolone and suplatast tosilate, following by just treatment with ST. Fourteen months after therapy and during maintenance treatment with ST, his symptoms had not recurred. (12)
Researchers in China shared a case study of a 56 year old male with gross hematuria and EC. In his case, oral prednisone with a slow tapering regiment was used, which achieved complete relief of EC symptoms at six months. This patient also had hypereosinophilic syndrome (HES)(13).
Researchers in Australia shared a similar case report, of a 56 year old woman with EC who was treated with one month of intravesical (bladder instillations) hydrocortisone and oral lortadine (antihistamine). They reported vast improvement in bladder lessons after treatment. (14)
As a last resort, some EC patients must have the affected area of the bladder removed (partial cystectomy).
Self-Help
Diet
From diet management to reducing muscle tension, patients can have a great deal of influence over their daily symptoms. As with several other bladder conditions, patients should understand that their bladder walls are incredibly inflamed and/or bleeding. Thus, reducing foods that can be irritating to those wounds, specifically acidic and/or caffeinated foods (citrus juices, sodas, artificial sugars, etc.) is essential. Food recommendations for interstitial cystitis apply to the EC patient as well. Learn more about bladder friendly foods here!
Hydration
Drinking adequate water every day is essential though difficult because many patients mistakenly assume that water is triggering their frequency. Urine contains toxins that your body is eliminating, such as urea. When urine is concentrated, it becomes much more potentially irritating to the bladder wall. It’s important to stay well hydrated, preferably with water or milk. Urine should be a pale, clear yellow. If it’s dark yellow or cloudy, then you’re dehydrated. If it’s clear, then you’re drinking too much water.
Heat or Cold Therapy
 The use of heat or cold packs over the bladder or perineum. IC patients often find heating pads very helpful in reducing muscle tension and/or discomfort. Microwavable pads work well for more severe flares. One time use, BodiHeat Pads, work well for driving, working and longer periods of time. Some patients also prefer cool packs especially to reduce a heat or burning sensation on the vulva or perineum.
The use of heat or cold packs over the bladder or perineum. IC patients often find heating pads very helpful in reducing muscle tension and/or discomfort. Microwavable pads work well for more severe flares. One time use, BodiHeat Pads, work well for driving, working and longer periods of time. Some patients also prefer cool packs especially to reduce a heat or burning sensation on the vulva or perineum.
OTC Supplements
OTC supplements have been found helpful for other bladder wall conditions, such as interstitial cystitis. There’s no evidence, though, that these can help with EC but they might be worth trying due, at a minimum, to the lower cost and risk of adverse events, including:
- Calcium glycerophosphate (aka Prelief) to reduce the acid in food.
- Phenazopyridine (Azo Bladder Pain Relief Tablets / Pyridium) for mild pain relief.
- Various nutraceuticals / OTC Supplements CystaQ, Cystoprotek and Desert Harvest Aloe
Meditation & Stress Management
Learning to relax and manage stress is a vital self-care strategy because stress is a well known pain trigger. The majority of patients report that their symptoms worsen during periods of high stress. Thus, taking a step back and looking at your overall stress levels as well as taking proactive steps to reduce stress is vital. Meditation is an excellent tool to use!
Muscle Relaxation & Guided Imagery
 Muscle tension is also a strong contributor to pelvic pain and bladder discomfort. During periods of high pain, muscles tighten in a “guarding reflex” that can then cause additional discomfort. Learning how to relax the pelvic floor muscles and muscles throughout the body is a key component to every successful pain management program. Luckily, three guided imagery CD’s are now available specifically for use in patients with pelvic pain.
Muscle tension is also a strong contributor to pelvic pain and bladder discomfort. During periods of high pain, muscles tighten in a “guarding reflex” that can then cause additional discomfort. Learning how to relax the pelvic floor muscles and muscles throughout the body is a key component to every successful pain management program. Luckily, three guided imagery CD’s are now available specifically for use in patients with pelvic pain.
Support
Patients struggling with emotional symptoms, such as anxiety, depression and catastrophizing, are strongly encouraged to seek help from psychological professionals and/or support groups. Research studies have proven that patients who have solid spousal and family support have a far better long-term outcome than those who don’t. The ICN’s Emotional Health Center contains articles that discuss anxiety, depression, surviving the holidays and several inspirational columns by author Frannie Rose. We also have s a discussion forum specifically for patients with EC. Find it in the ICN Support Forum!
References
- Eosinophilic Cystitis. Office of Rare Diseases Research. National Center for Advancing Translational Sciences. June 2, 2011
- Eosinophil Associated Disorders Fact Sheet, American Partnership of Eosinophilic Disorders – Updated 6/1/11
- Kojima K, et al. Eosinophilic cystitis presented as a manifestation of hypereosinophilic syndrome: a case report and review of the literature. Nephron Extra 2013 Jan;3(1):30-5
- D M, et al. Eosinophilic cystitis mimicking bladder tumour – a rare case report. J Cli. Diag Res. 2013 Oct:7(10):2282-3
- Mallat F, et al. Eosinophilic cystitis with eosinophilic cholecystitis: a rare association. Case Rep Urol. 2013:146020
- Muraoka K, et al. Eosinophilic cystitis caused by Sijo-bohhu-tou: a case report. Hinyokika Kyo 2009 Jun;55(6):353-5
- Venkatesh KS, et al. Eosinophilic cystitis: a rare cause of hematuria in children. Case Rep Nephrol 2012:710230
- Guerra LA, et al. Pseudo-tumoral eosinophilic cystitis in a 3 year old girl. Can J Urol. 2005 Oct;12(5):2846-8
- Rossi E et al. Eosinophilic cystitis and nephrogenic adenoma of the bladder: a rare association of 2 unusual findings in childhood. J Pediatric Surg 2011 Apt;46(4)
- Galutira PJ, et al. Presenting manifestations of eosinophilic cystitis in two Filipino Children. Int Urol Nephrol 2010 Sept;42(3);557-63
- Yu S, et al. Montelukast as a successful treatment for eosinophilic cystitis in an asthmatic woman patient. Pak J Med Sci. 2013 Sep;29(5):1280-2.
- Yoshino T, et al. Case of eosinophilic cystitis treated with suplatast tosilate as maintenance therapy. Case Rep Urol. 2013:354219
- Jiang P, et al. Eosinophilic cystitis in a patient with hypereosinophila syndrome: A case report. Exp Ther Med. 2014 Jul;8(1):49-51. Epub 2014 May 12.
- Zaman SR. Eosinophilic cystitis: treatment with intravesical steroids and oral antihistamines. BMJ Case Report: 2013 Sep 6; 2013
- Book W. Eosinophilic Cystitis. American Partnership For Eosinophilic Disorders, August 30, 2011
- Teegavarapu PS, et al. Eosinophilic cystitis and its management. Int J Clin Pract. 2005 Mar;59(3):356-60.

