In our introduction, you learned that most IC patients have an injured bladder wall in the form of glomerulations or Hunner’s Ulcers/Lesions. As the bladder fills, urine enters these wounds where it causes irritation and inflammation, triggering the symptoms of frequency, urgency and/or pain. From a treatment standpoint, your goal is to promote healing in your bladder. Some medications fight inflammation while others provide a “bandaid” like effect. The foundation of success, however, often lies in the simple self-help strategies that you can and should be doing each day. From avoiding foods which irritate the bladder to simple muscle work, you do have the power, each day, to help yourself. I’ll be exploring self-help strategies in our next tour stop! In the meantime, let’s talk about bladder treatments! – Jill Osborne, ICN President & Founder
In 2011, the AUA released a six step guideline for the treatment of IC/BPS. Improving YOUR quality of life should be the first goal of therapy. As various treatments are considered, you and your physician should consider the risk of side effects and adverse events. As a rule, the AUA suggests that treatment should begin with generally safe “conservative” therapies, such as oral medications and simple bladder instillations. If no improvement occurs, “less conservative” treatments that have more risk of side effects and adverse events can be explored, such as neuromodulation and Botox. Surgery is rarely utilized and only under specific circumstances because it is irreversible.
It is important for you and your clinicians to track the progress of each treatment, usually with a voiding diary. The ICN Medical Records Kit also provides tracking tools. The AUA states that ineffective treatments should be stopped after a “clinically meaningful interval.” Only effective treatments should be continued. If a patient has not shown improvement in their symptoms after multiple treatments, they suggest that the diagnosis of IC should be revisited to determine if another underlying disorder (i.e such as pudendal nerve entrapment, endometriosis, etc.) is present.
The AUA also encourages prompt and proactive pain treatment. They offered “Pain management should be continually assessed for effectiveness because of its importance to quality of life.” Pain management can include the use of various medications, physical therapy and/or the relaxation of tense, painful muscles, biofeedback and a wide variety of other options. The guidelines encourage physicians to refer patients to other pain specialists if they are unable to provide an effective pain management strategy.
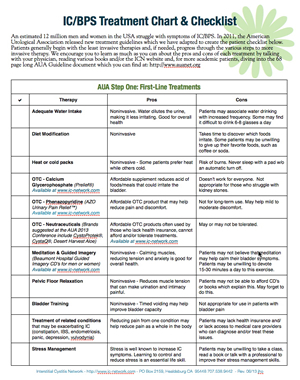
Read the ICN Summary of the AUA treatment recommendations (2 pages)
Read the full AUA Guidelines (68 pages)
Video Presentation of Guidelines
Here is a video produced by the American Urological Association, featuring Dr. Phil Hanno (UPENN) discussing the new guidelines.