Many Patients With Fibroids Struggle With Bladder Symptoms
Have you struggled with urinary symptoms that aren’t responding to traditional bladder treatments? Do you also struggle with painful cramping and/or intense bleeding? Uterine fibroid tumors (aka leiomyomas) might be a hidden source of your symptoms. A new research study has shown that when fibroid tumors are reduced in size and/or removed, urinary symptoms can improve dramatically. In fact, 97% of the patients in this study had urinary symptoms and 65% were “cured” of their urinary symptoms once the fibroids were treated.1
What are fibroids?
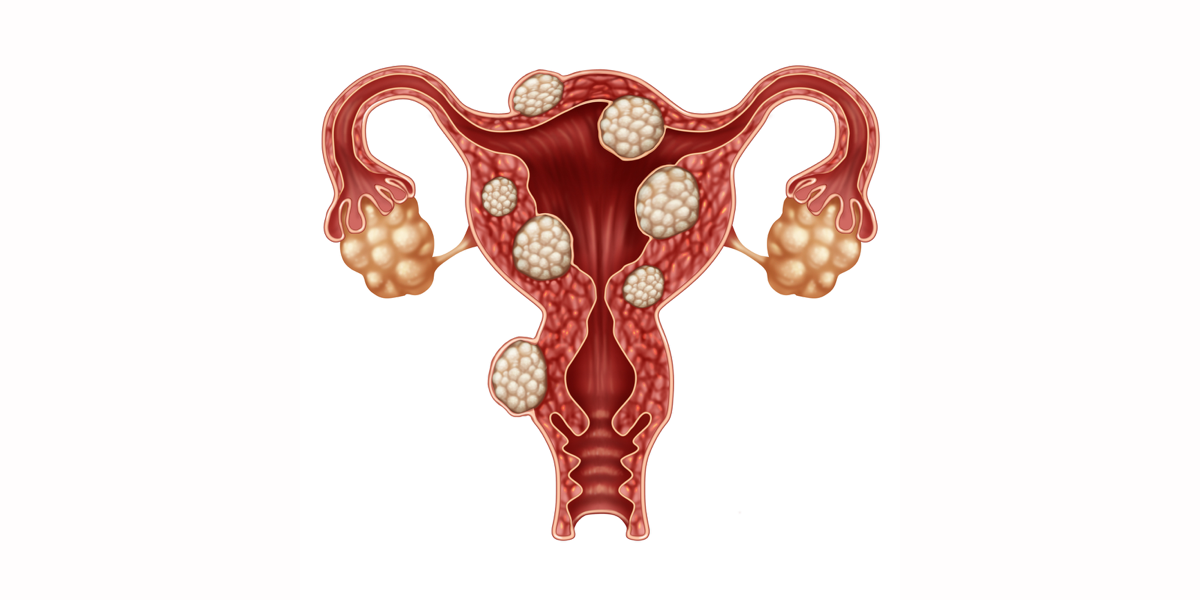
Millions of women struggle with fibroid tumors, non-cancerous growths that can grow inside the uterus, within the uterine wall or outside of the uterus. They can occur as a single tumor or in clusters. They can be so small they are invisible to the naked eye or so large and heavy that they distort the size of the uterus and put pressure on the bladder and/or rectum.
ICN member ICshorty said “I had such big fibroids that I looked fairly pregnant & had to lift my uterus off of my bladder in order to void…” Christina P shared “I have a large fibroid I am planning on having removed as it is tilting my uterus and putting pressure on my bladder.”
The UCLA Fibroid Treatment Center estimates that 60 to 80% of women may develop fibroids by the time they reach age 50.(2) Most have no idea that they have fibroids because they often cause no symptoms. However, about 20% of patients struggle with symptoms, often heavy menstrual bleeding that can lead to anemia and longer periods.
If a fibroid is pressing against the bladder, it can mimic many of the symptoms of IC, including urinary frequency, sleeplessness, nocturia, and difficulty starting urination. Fibroids can also trigger kidney dysfunction. “When they’re [fibroids] quite large they can put pressure on the tubes that take the urine from the kidney to the bladder and they actually cause the kidney to enlarge,” said Dr. Charles Miller, the division director of minimally invasive gynecologic surgery at Advocate Lutheran General in Park Ridge, Illinois.(3) Fibroids close to the rectum may cause rectal pressure, fullness and/or constipation. If a fibroid is pressing against the bladder, it can mimic many of the symptoms of IC, including urinary frequency, sleeplessness, nocturia, and difficulty starting urination.
Large, growing fibroids can trigger pelvic pain and pressure. Patients frequently report a heaviness in the pelvic area or might even feel a large mass when they press into their lower abdomen. They can become so large that the patient may look pregnant. Just last year, a 61 pound fibroid resembling a pumpkin was removed from a 53 year old woman in Singapore.(4)
Fibroids can also influence fertility and trigger miscarriages. They can block fallopian tubes, which can make it difficult for a fertilized egg to drop into the uterus. It can be difficult for an embryo to attach to the uterine wall. Large fibroids can even restrict the growth of a fetus.
Risk Factors
Fibroids are more common as women age, especially during the 30’s and 40’s. Patients with family members with fibroids have more risk. If your mother had fibroids, your risk of having them is higher. High blood pressure, vitamin D defi- ciency and no history of pregnancy may be risk factors. In contrast, preg- nancies appear to reduce the risk of fibroids.(5)
One preventable risk factor for fibroids is obesity. Very heavy women have 2 to 3x the risk of developing fibroids.(6) Women who carry excess fat in the abdominal area and have a body fat percentage over 30% are at increased risk for fibroids.(7)
Why the connection? Researchers suspect that obesity is linked to high rates of circulating estrogen.(8) These patients have less serum hormone- binding globulin (SHBG) proteins which allow more estrogen to circulate. Obesity can also disrupt communication between cells in the uterine wall which can also trigger abnormally high estrogen levels.(9) Though menopause often triggers the reduction in fibroids due to the cessation of estrogen production by the ovaries, the excess belly fat we can develop may produce excess estrogens that can circulate through the body and to the uterus.10
Diagnosis
Uterine fibroids are often discov- ered during routine gynecological exams or ultrasound. To the physician, they can feel like a hard lump during the pelvic exam. Doctors may then order a variety of tests including ultrasound, MRI, hysterosonogram, hysterosalpingogram or hysteroscopy.
Treatment
As with interstitial cystitis, medical care providers encourage patients to begin with the least invasive methods first, with a healthy of dose of good nutrition, self-help and stress management thrown in.
Diet Modification
Many foods contain estrogens that could also trigger fibroid growth. The Fibroid Treatment Collective encourages an anti-estrogen diet instead(11), including:
- Cruciferous vegetables – broccoli, cabbage, bok choy, kale, turnips, watercress, radish and arugula are all great choices. Avoid overcooking these vegetables so that they retain most of their nutrients.
- Garlic, carrots, beets and drinking plenty of water.
- Foods that contain carotenes – Apricots, sweet potato, cantaloupe, carrots, pumpkin and spinach are all sufficient sources.
- Foods containing vitamin E – like almonds, wheat germ, hazelnuts and cod liver oil.
- Natural anti-inflammatory foods – pineapple and fresh rosemary have been shown to help decrease inflammation.
- Polyphenol, which is found in green tea, can help to counteract the effects of estrogen. Unfortunately, this can irritate a sensitive bladder.
They suggest eliminating the following foods that may increase estrogen levels:
- Red meat, alcohol, animal fats, cheese, cream, butter, ice cream and chocolate have all been shown to raise levels of estrogen. The fat from turkey and chicken should also be trimmed before cooking.
- Low-fat milk should be swapped for whole milk.
- Artificial sweeteners
- Soy products
- Avoid storing food in plastic containers.
Weight Loss
If you follow the diet suggestions above, weight loss is likely and for the obese patient, it can help dramatically. One study found that patients who lost weight with diet modification and exercise had an 11.9% reduction of estrogen levels. SHBG levels also increased by 25.8%.(12)
Oral Medications
Medications that regulate hor- mones may help reduce symptoms.(13) Androgens (medications similar to testosterone) stop menstruation and may shrink tumors and reduce the size of the uterus. Unfortunately, they can also cause weight gain, depres- sion, anxiety, acne, headaches and unwanted hair loss. Oral contracep- tives (birth control pills) can help control bleeding.
Lupron, a medication that blocks the production of estrogen and progesterone, puts the patient into a temporary menopause and can cause fibroids to shrink. This is often used before surgery to help reduce the size of the tumors and to resolve anemia that could lead to blood transfusions during surgery. The challenge of this type of medication is that the patient can also experience other symptoms of menopause such as hot flashes.
Minimally Invasive Procedures
If oral therapy does not work, minimally invasive procedures may be suggested. A progestin-releasing IUD can relieve heavy bleeding but does not reduce the size of the fibroids.(13) Uterine artery embolization cuts off blood flow to fibroids yet pre- serves the uterus and is recom- mended for women who would like to have more children.
The newest treatment method that involves neither knife nor needle is MR Guided Focused Ultrasound. It is a completely non-invasive treatment for small to medium size fibroids that uses high intensity focused ultrasonic waves to destroy the fibroid tissue. It is done as an outpa- tient procedure, with conscious sedation.(13)
Surgical Procedures
Patients would who like to keep their uterus and/or who wish to bear more children often select a hysteroscopic myomectomy. Performed through a hysteroscopy (instruments are inserted through the vagina and cervix), a surgeon may be able to easily remove fibroids that are shallow and located near the surface of the uterus (i.e submucosal). Laparoscopic and robotic myomectomy surgery can be used to also remove medium sized fibroids, in this case through the abdominal wall. This may save the uterus and has a rapid recovery time when compared to open surgery. Large fibroids or fibroids in difficult locations may require removal through the abdominal wall. Larger incisions and general anesthesia usually require a longer recovery time. Hysterectomy is the last resort for patients with the most severe cases.
Conclusion
If you struggle with painful periods, pelvic pressure, bladder pressure, nocturia, constipation, you should ask your physician if fibroid tumors could be contributing to your symptoms. The AUA Guidelines are crystal clear in their suggestion that IC patients who are not responding to therapy and/or who are worsening overtime have a new diagnostic assessment. Was something missed? Could that patient have pelvic floor dysfunction? Hunners’ lesions? Chronic UTI? Candida? Fibroids should be added to the list of condi- tions to be ruled out.
References
- Houlihan S, et al. Fibroid surgery and improvement in bladder symptoms; The FAB study. Neurourology and Urodynamics. Vol. 37. Issue 6. August 2018
- UCLA Fibroid Symptoms Treatment and Diagnosis. Accessed 2/14/19. http://obgyn.ucla.edu/fibroids
- Harris, Collette. Eight silent signs you have uterine fibroids. Readers Digest Health. Accessed 2/14/19 – https://www.rd.com/health/conditions/fibroid-symptoms/
- Nierenberg, C. Pumpkin-size giant fibroid removed form woman’s uterus. Live Science. September 7, 2018.
- What are the risks for uterine fibroids. NICHD Publication. 11/2/2018
- US Dept of Health and Human Services, Office on Women’s Health. (2015). Uterine Fibroids Fact Sheet.
- Khan, A. T., Shehmar, M., & Gupta, J. K. (2014). Uterine fibroids: current perspectives. International Journal of Women’s Health, 6: 95-114.
- Sarwer D, et al. Sexual functioning and sex hormones in persons with extreme obesity and seeking surgical and non-surgical weight loss. Surgery for Obesity and Related Diseases 2013: 9(6).
- He Y, et al. Associations between uterine fibroids and lifestyles including diet, physical activity and stress: a case-control study in China. Asia Pacific Journal of Clinical Nutrition, 2013: 22(1): 109-117.
- Van den Bosch T, et al. Screening for uterine tumors. Best Practice & Research Clinical Obstetrics & Gynaecology, 2012: 26(2): 257-266.
- Foods and Fibroids: Should I Follow a Diet Plan. Fibroid Treatment Collective. August 3, 2017. https://fibroids.com/blog/food-fibroids- follow-diet-plan/
- Campbell KL, et al. Reduced-calorie dietary weight loss, exercise, and sex hormones in postmenopausal women: randomized controlled trial. Journal of Clinical Oncology, 2012: 30(19): 2314-2326.
- UCLA Fibroid Treatment Options. Accessed 2/14/19. http://obgyn.ucla.edu/medical-therapy.jspFibroids
Reprinted from the IC Optimist Magazine, Winter 2019 edition